Ozempic, Zepbound, and Oral Health: Side Effects Dentists Are Watching
Are your weight loss medications affecting your smile?
Medications like Ozempic, Wegovy, Saxenda, Mounjaro, and Zepbound have become household names in the treatment of obesity and type 2 diabetes. But while these GLP-1 receptor agonists offer impressive results for weight loss and blood sugar control, their impact on oral health is less discussed—yet potentially significant.

- Dry Mouth (Xerostomia)
Dry mouth is not an officially listed side effect for all GLP-1 drugs, but many users—especially those on tirzepatide (Zepbound, Mounjaro)—report this uncomfortable symptom.
- Why it happens: GLP-1 medications can reduce saliva production by altering hormone regulation. Nausea, vomiting, and decreased fluid intake (due to suppressed appetite) can also contribute to dehydration.
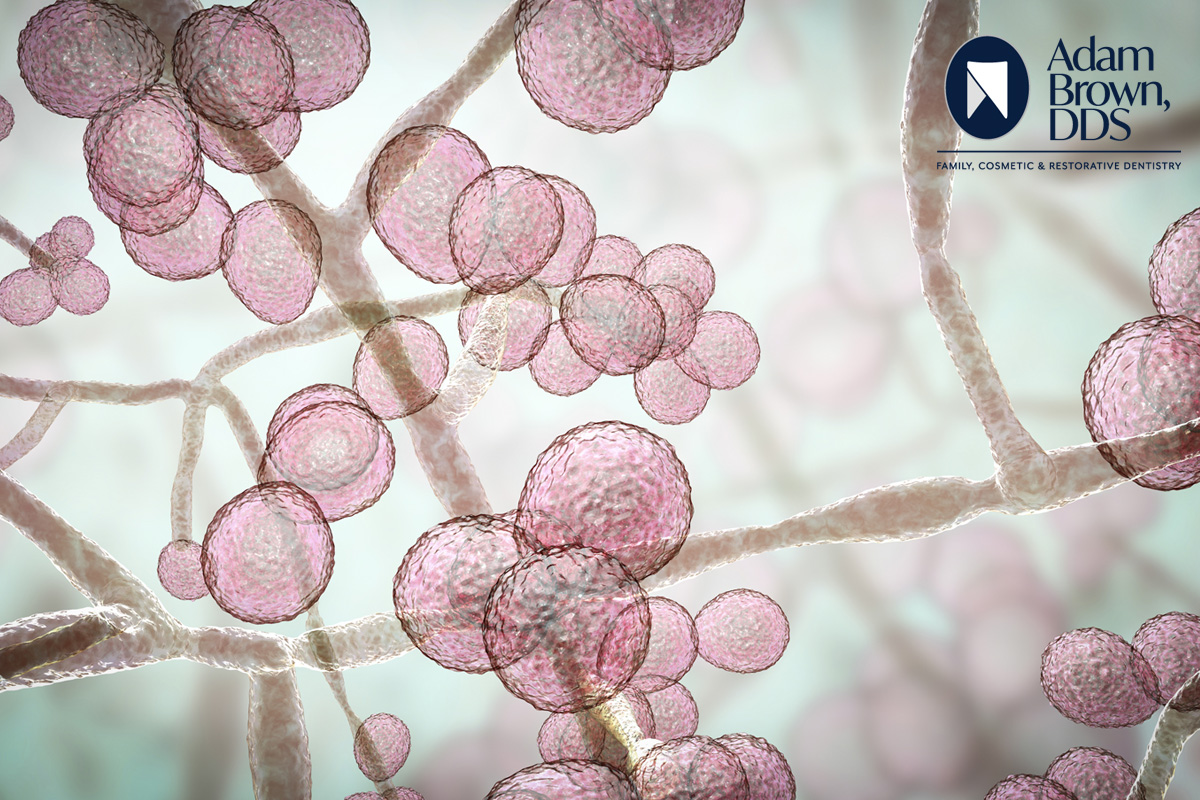
- Oral impact: A dry mouth increases the risk for tooth decay, gum disease, bad breath, and oral infections such as candidiasis.
(Sources: Drugs.com, Well Wisp, Drugs Coverage)
- Nausea and Vomiting
These are among the most common side effects of GLP-1 drugs, particularly during the first few weeks or dose increases.
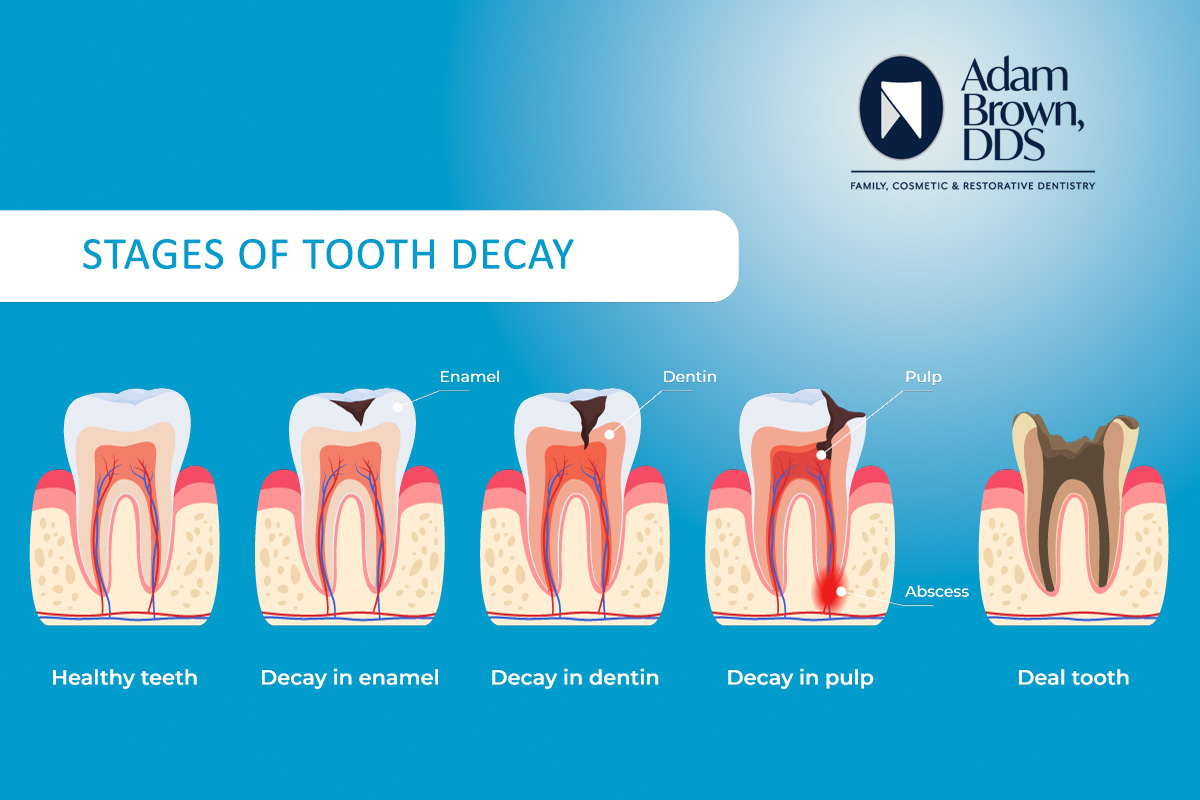
- Oral impact: Frequent vomiting exposes teeth to stomach acid, which can erode enamel, increasing the risk for cavities, sensitivity, and enamel thinning.
- Altered Taste Sensation (Dysgeusia)
Some patients on Zepbound and similar medications report a persistent metallic or bitter taste, even when not eating.
- Possible cause: It’s believed that the drug may circulate in saliva and interact with taste receptors.
- Oral impact: Changes in taste can make eating less enjoyable and may lead to decreased food variety or poor oral intake.
- Tooth Damage and Loss
There have been anecdotal reports of significant dental issues from users of tirzepatide, including chipped, cracked, or lost teeth.
- Suspected link: Rapid weight loss, nutritional deficiencies (especially calcium or vitamin D), and possible changes in bone density could compromise oral structures.
- Note: These cases are rare and not conclusively proven to be caused by the medication, but they warrant attention.
(Sources: Drugs.com, The Sun)
- Mouth Ulcers
Though not commonly reported, some users of Zepbound and Mounjaro have noted painful mouth sores or ulcers.
- Possible mechanism: Reduced saliva flow can make the oral environment more prone to irritation and tissue breakdown.
(Source: Drugs Coverage)
- Diet-Related Effects
GLP-1 drugs significantly alter appetite and often reduce intake of sugar and processed foods.
- Oral benefit: Less sugar means lower cavity risk.
- Potential drawback: If nutrient intake becomes too restricted—especially calcium, vitamin D, and protein—this could negatively affect jawbone health, gums, and healing capacity.
- Acid Reflux or GERD
GLP-1 medications slow gastric emptying, which can worsen acid reflux in some individuals.
- Oral impact: Stomach acid reaching the mouth can erode tooth enamel and contribute to increased sensitivity and decay over time.
What This Means for Patients
If you’re taking a GLP-1 medication like Zepbound and noticing changes in your mouth—such as dryness, bad taste, tooth sensitivity, or ulcers—don’t ignore them. These effects may seem mild but can lead to serious dental problems if left unaddressed.
Recommendations for Protecting Oral Health While Taking GLP-1 Medications
If you’re using a GLP-1 drug like Zepbound, Ozempic, or Mounjaro and are concerned about your oral health, there are proactive steps you can take to protect your teeth and gums:
- Stay Well-Hydrated: Drink plenty of water throughout the day to help relieve dry mouth and support saliva production.
- Stimulate Saliva Naturally: Chew sugar-free gum or suck on sugar-free lozenges to keep your mouth moist.
- Practice Excellent Oral Hygiene: Brush at least twice a day, floss daily, and consider using a fluoride toothpaste or mouth rinse to help strengthen enamel.
- Be Gentle After Vomiting: If nausea leads to vomiting, avoid brushing immediately afterward. Instead, rinse your mouth with water or a baking soda solution to neutralize stomach acid and protect your enamel.
- Monitor for Symptoms: Watch for changes in taste, increased sensitivity, mouth sores, or visible tooth damage—and don’t ignore subtle warning signs.
- Schedule Regular Dental Visits: Make sure to keep up with cleanings and checkups. Let your dentist know you’re taking a GLP-1 medication so they can look for related issues.
- Talk to Your Healthcare Team: If you notice any new or worsening oral symptoms, discuss them with both your dentist and your prescribing physician. Adjustments to your treatment plan or additional support may be helpful.
While clinical research on the oral side effects of GLP-1 medications like tirzepatide (Zepbound) is still emerging, these real-world experiences emphasize the importance of staying proactive about your dental care during treatment.



 Research was led by Dr. Damien Brady, whose team set out to find out if the coconut oil would have an effect on the bacteria Streptococcus, which is present in virtually all human mouths. It is the Streptococcus that is responsible for almost all instances of tooth decay in humans. These bacteria break down sugars consumed and produce acid that wears out teeth. The wearing, in turn, becomes decay.
Research was led by Dr. Damien Brady, whose team set out to find out if the coconut oil would have an effect on the bacteria Streptococcus, which is present in virtually all human mouths. It is the Streptococcus that is responsible for almost all instances of tooth decay in humans. These bacteria break down sugars consumed and produce acid that wears out teeth. The wearing, in turn, becomes decay.