Symptoms, Management, and Treatment of Oral Thrush – How to Reduce Your Risk- Naturally
What is thrush?
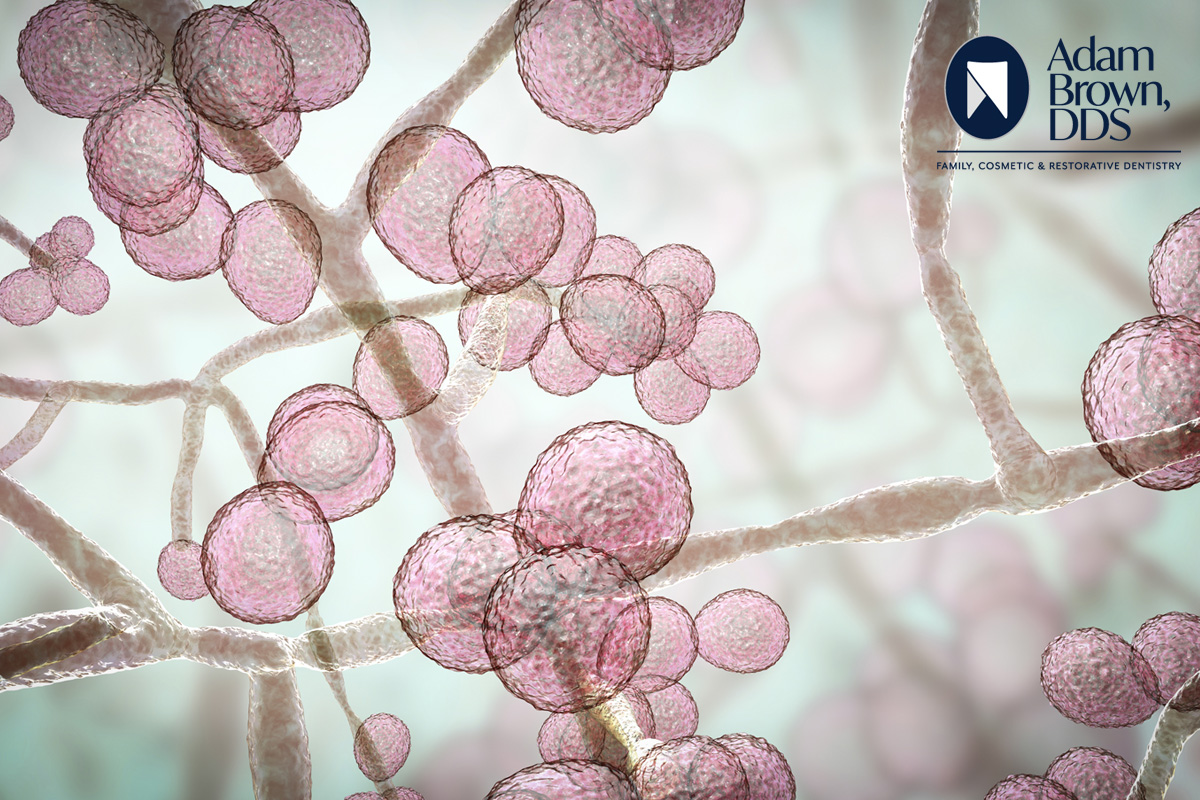
Thrush is a fungal (yeast) infection that grows in mouths, throats and other parts of the body. Oral thrush presents symptoms including white, raised lesions (looking a bit like cottage cheese) on tongues and cheeks. This condition can become irritated and soon cause redness and mouth pain.
The Cleveland Clinic shares, “Candida albicans is a fungus that lives on your body in small amounts, located in your mouth, skin and intestines. Candida is a yeast that is responsible for infections like thrush if it is off-balance with healthy bacteria in your body. Infections are common and treated with antifungal medications.”
Many new parents have been concerned and confused over the diagnosis that their baby has thrush. Babies under 1 month old and toddlers (as well as adults over 65 and those with weakened immune systems) are at a higher risk of getting thrush. Babies’ and toddlers’ immune systems are still developing, thus the higher risk. St. Louis (MO) Children’s Hospital reports 5% of infants develop thrush. See your child’s pediatrician if you see symptoms of thrush.
The Mayo Clinic offers, “If you’re breastfeeding and your infant has oral thrush, you and your baby could pass the infection back and forth. Your doctor may prescribe a mild antifungal medication for your baby and an antifungal cream for your breasts.”
Symptoms
Thrush can happen fast with a sudden development of symptoms. Most commonly: the presence of creamy white, slightly raised lesions in your mouth (usually on your tongue and inner cheeks), you might also have lesions on the roof of your mouth, gums, tonsils or the back of your throat.
Some patients report soreness and redness inside and at the corners of the mouth, loss of taste and a “cottony” feeling (dry mouth).
Lesions may hurt and bleed a bit when you brush your teeth or rub against them. In severe cases, lesions can spread into the esophagus and cause painful swallowing, or fever.
Cleveland Clinic warns, “Thrush can spread to other parts of your body, including your lungs, liver and skin. This happens more often in people with cancer, HIV or other conditions that weaken the immune system.”
It’s important to act when symptoms appear.
What can cause thrush in adults?
“Most people have small amounts of the Candida fungus in their mouth, digestive tract and skin. When illnesses, stress or medications disturb this balance, the fungus grows out of control and causes thrush” shares the Cleveland Clinic. Medications that can make yeast flourish and cause infection include: corticosteroids, antibiotics, and birth control pills.
While thrush can be contagious for those with at-risk conditions, like weakened immune systems, for people with healthy immune systems, it’s rare to pass thrush along via kissing or close contact. If you are worried about catching it, avoid the infected person’s saliva. And with most illnesses, it’s always wise to wash your hands properly and often.
Some risk factors for developing thrush include diabetes, anemia, HIV/AIDS, cancer, dry mouth (xerostomia), pregnancy, smoking and ill-fitting dentures.
If you have concerns about your dentures fitting correctly, reach out to the Adam Brown, DDS team.
Beware of Complications.
Though thrush rarely causes complications in those with healthy immune systems, those with weakened immune systems can potentially get infections from Candida entering the bloodstream. It can spread to other areas of your body including the heart, brain, and eyes or lead to septic shock. If you are in a high-risk group, see your physician as soon as possible.
How is thrush diagnosed?
From the Cleveland Clinic, “A healthcare provider can usually tell right away if you have thrush by looking for the distinctive white lesions on your mouth, tongue or cheeks. Lightly brushing the lesions away reveals a reddened, tender area that may bleed slightly. A microscopic exam of tissue from a lesion can confirm whether or not you have thrush.”
If thrush extends into your esophagus, your healthcare provider might:
- Take a throat culture (swab the back of your throat with sterile cotton and study microorganisms under a microscope).
- Perform an endoscopy of your esophagus, stomach and small intestine (examine the lining of these areas with a lighted camera mounted on the tip of a flexible tube).
- Take X-rays of your esophagus.
Management and Treatment
The typical treatment for thrush is antifungal medications prescribed by your healthcare provider. These medications are available in tablets, lozenges and sometimes liquids that are “swished” around before swallowing. The typical length of treatment is 10-14 days. The type of treatment recommended will be specific to your age and the cause of the infection.
Kids and adults with healthy immune systems typically respond well to antifungal treatment. But thrush symptoms may be more severe and harder to treat in those with weakened immune systems. Refer to the potential complications listed earlier. For most, thrush will clear up in 1-2 weeks.
If you’ve already taken antifungals for thrush but your symptoms return, call your healthcare provider right away. It could indicate a more serious infection.
Tips for Prevention: Crush Thrush!
You can do these things to reduce your risk for thrush:
- Practice good oral hygiene. Brush your teeth at least twice a day and floss at least once a day. If you have any questions about this, our team is a quick call away at 704-289-9519.
- Avoid certain mouthwashes or sprays. Some of these products can destroy the normal balance of microorganisms in your mouth. Talk to Adam Brown, DDS or your doctor about which ones are safe to use.
- See your dentist regularly. This is especially important if you have diabetes or wear dentures. At Adam Brown, DDS, we want you to know that our goal is to keep your mouth healthy! If you need to make an appointment, our team is ready to help at 704-289-9519 or use our convenient “schedule an appointment” option and we’ll call you to set up a time to come in for a check-up or whatever else you may need.
- Limit the amount of sugar and yeast-containing foods you eat. Foods such as bread, beer and wine encourage Candida growth.
- Avoid smoking and other tobacco use. Ask your healthcare provider about ways to help you quit smoking (and vaping). Smoking tobacco can be very damaging to your oral health, people who smoke are at higher risk of developing oral (mouth) cancer, tooth loss, root decay and complications after procedures.
Home Remedies
Ultimately, you’ll need antifungal medication to clear up thrush. These come in the form of mouthwashes, pills or lozenges.
Mild cases of oral thrush may go away on their own.
The following is a selection of home remedies that, when used in addition to antifungal medications, may help relieve symptoms of the infection (shared from www.healthline.com).
- Salt water
Salt has antiseptic, cleansing, and soothing properties, making it a common home remedy for many oral problems.
Rinsing your mouth with salt water could help relieve symptoms of oral thrush.
To use:
- Dissolve 1/2 teaspoon salt in 1 cup warm water.
- Swish the solution throughout your mouth.
- Spit out the salt solution.
- Baking soda
Rinsing your mouth with baking soda (sodium bicarbonate) may help treat oral thrush.
In 2021, research focused on the use of sodium bicarbonate to treat thrush.
To use:
- Dissolve 1/2 teaspoon of baking soda in 1 cup warm water.
- Swish the rinse throughout your mouth.
- Spit out the rinse.
- Yogurt
Probiotic yogurt contains live, “good” bacteria cultures that may treat oral thrush.
The cultures don’t kill Candida. Instead, they stop its growth. They may also help restore the proper balance of good to bad bacteria in the mouth.
Since it’s soft, yogurt is also a great food to eat if you’re having trouble swallowing due to painful mouth and throat lesions.
To use:
- Eat yogurt a couple times daily at the first sign of oral thrush.
- Choose unsweetened varieties of yogurt since Candida thrives on sugar.
- If you don’t like yogurt, you can get the same benefits by taking a daily probiotic supplement.
- Lemon juice
Lemon juice is thought to have antiseptic and antifungal abilities that help it fight against the fungus that causes thrush.
Lemon juice was found to be an effective treatment for oral thrush.
To use:
- Add the juice of half a lemon to 1 cup warm or cool water.
- Drink the mixture or use it as a mouth rinse.
Some people apply lemon juice directly to thrush lesions, but the lemon’s acidity may cause burning and irritation.
- Apple cider vinegar
People with dentures have a higher risk of oral thrush. Dentures that don’t fit properly or that aren’t cleaned well provide the ideal environment for Candida to thrive. This may cause a condition similar to thrush called denture stomatitis. Apple cider vinegar has antifungal properties.
Please contact the team at Adam Brown, DDS if you have any concerns about the proper fit of your dentures.
To use:
- Add 1 teaspoon raw, unfiltered apple cider vinegar to 1 cup water.
- Swish the rinse throughout your mouth for at least 15 seconds.
- Spit out the mixture.
If you rinse with undiluted apple cider vinegar, be aware that this may cause a painful burning sensation in your mouth.
- Vitamin C
Vitamin C (also called ascorbic acid) is necessary for proper immune system function. It does this by encouraging white blood cell production, which helps protect your body against infection.
It also helps these cells function more effectively and protects them against harmful molecules.
A healthy immune system helps bring balance back to your body. Increasing your intake of vitamin C if you’re deficient may help boost your body’s immune system to fight the infection.
Questions or concerns about being diagnosed with thrush? Contact Adam Brown, DDS or your healthcare provider. Together, we can “crush thrush” and you’ll be feeling better so