Understanding the Metallic Taste: Common Causes
Experiencing a metallic taste in your mouth, medically known as dysgeusia, can be both perplexing and unpleasant. This condition can affect your enjoyment of food and overall quality of life. Understanding the potential causes and exploring effective home remedies and preventive measures can help alleviate this issue.

Understanding the Metallic Taste: Common Causes
A metallic taste can arise from various factors, ranging from lifestyle habits to underlying medical conditions. Here are some prevalent causes:
- Poor Oral Hygiene
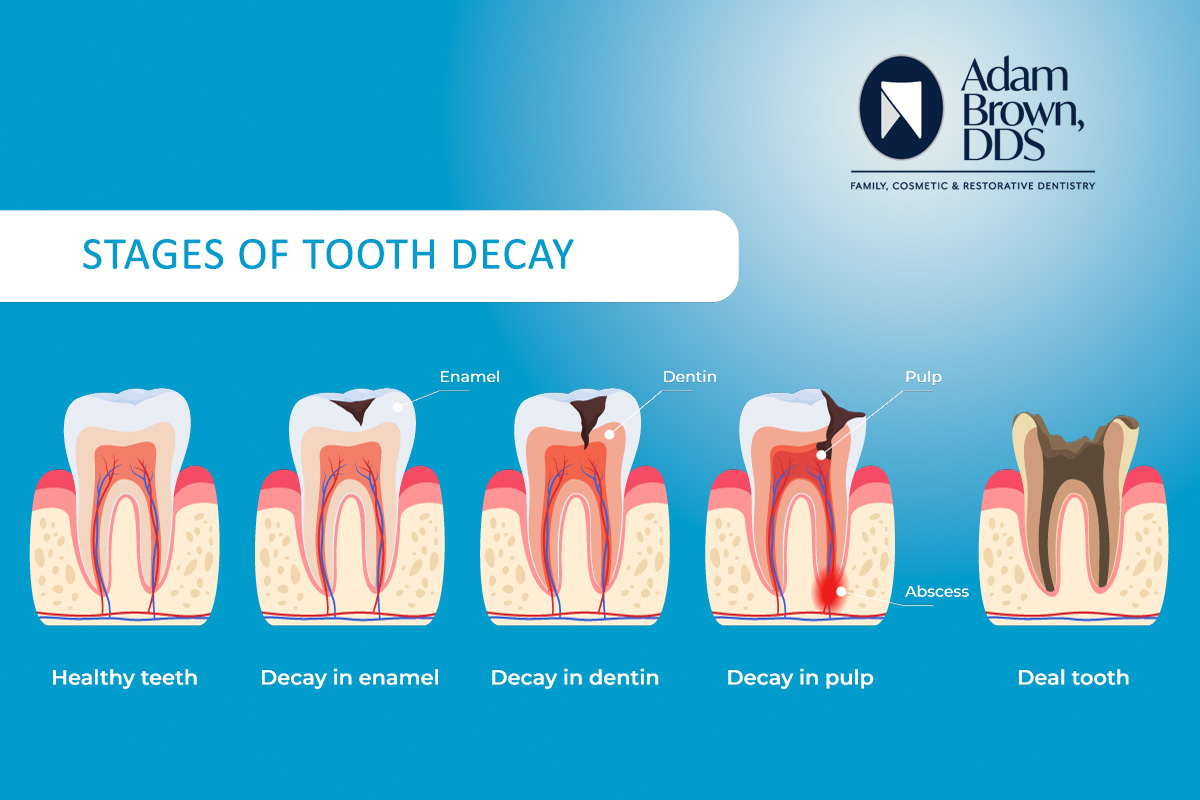
Inadequate brushing and flossing can lead to dental problems such as gingivitis, periodontitis, and tooth infections. These conditions can contribute to a metallic taste in the mouth. Maintaining proper oral hygiene is essential to prevent such issues.
Medical News Today
- Medications
Certain medications are known to cause a metallic taste as a side effect. These include antibiotics like clarithromycin and metronidazole, blood pressure medications such as captopril, and medications like metformin used to treat diabetes. The body absorbs these drugs, and they can be excreted into the saliva, leading to taste disturbances.
- Over-the-Counter Vitamins and Supplements
Multivitamins containing heavy metals like chromium, copper, and zinc, as well as prenatal vitamins and iron or calcium supplements, can cause a metallic taste. This typically occurs as the body processes these substances.
- Infections
Upper respiratory infections, colds, and sinusitis can alter your sense of taste, resulting in a metallic sensation. These changes are usually temporary and resolve once the infection clears.
- Cancer Treatments
Patients undergoing chemotherapy or radiation therapy, especially for head and neck cancers, may experience taste changes, including a metallic taste. This phenomenon is sometimes referred to as “chemo mouth.”
- Pregnancy
Hormonal fluctuations during pregnancy can lead to dysgeusia, causing expectant mothers to experience a metallic or sour taste. This symptom is typically most pronounced during the first trimester and often diminishes as the pregnancy progresses.
- Neurological Conditions
Neurological disorders, such as dementia, can affect taste perception, potentially leading to a metallic taste. This occurs due to the degeneration of taste buds and changes in the way the brain interprets taste signals.
Home Remedies to Alleviate Metallic Taste
If you’re experiencing a metallic taste, several home remedies may help mitigate the sensation:
- Maintain Good Oral Hygiene
Brush your teeth and tongue at least twice a day and floss daily. This practice helps remove food particles and bacteria that can contribute to taste disturbances.
- Rinse with Baking Soda Solution
Rinsing your mouth with a solution of half a teaspoon of baking soda and half a teaspoon of salt dissolved in one cup of warm water before meals can neutralize acids and reduce a metallic taste.
- Stay Hydrated
Drinking plenty of water helps keep your mouth moist and can wash away substances that might be causing a metallic taste.
- Chew Sugar-Free Gum
Chewing sugar-free gum or sucking on sugar-free candies can stimulate saliva production, which may help wash away the metallic taste.
- Use Plastic Utensils
Using plastic utensils instead of metal ones can help reduce the metallic taste, especially if it’s triggered by contact with metal cutlery.
- Adjust Your Diet
Incorporate naturally sweet foods, such as citrus fruits, to help mask a metallic taste. For example, adding a spritz of orange to foods and drinks can be beneficial.
- Quit Smoking
Smoking can dull your sense of taste and contribute to a metallic sensation. Quitting smoking can improve your overall oral health and taste perception.
- Avoid Metal Cookware
Cooking with glass or ceramic cookware instead of metal pots and pans can help prevent a metallic taste in your food.
- Marinate Meats
Marinating meats in sweet fruit juices or sweet wines, or cooking with plenty of herbs and spices, can help mask a metallic taste.
Preventive Measures
To reduce the likelihood of developing a metallic taste in your mouth, consider the following preventive strategies:
- Regular Dental Check-Ups
Visit your dentist regularly for check-ups and cleanings. Addressing dental issues promptly can prevent infections that might lead to taste disturbances.
- Manage Medications
If you suspect a medication is causing a metallic taste, consult your healthcare provider. They may adjust your dosage or suggest an alternative medication.
- Address Underlying Health Conditions
Managing chronic conditions such as diabetes, kidney disease, or liver disease can help prevent taste disturbances associated with these illnesses.
References:
- Medical News Today – www.medicalnewstoday.com (Covers oral hygiene and its link to taste disturbances)
- WebMD – www.webmd.com (Discusses causes, home remedies, and preventive measures for metallic taste)
- Sendhil Dental – www.sendhildental.com (Explains hydration’s role in reducing metallic taste)
- Harvard Health – www.health.harvard.edu (Provides dietary recommendations for managing taste disturbances)
- Oral-B – www.oralb.co.uk (Covers the impact of smoking on taste perception)


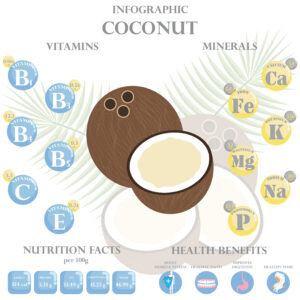 Research was led by Dr. Damien Brady, whose team set out to find out if the coconut oil would have an effect on the bacteria Streptococcus, which is present in virtually all human mouths. It is the Streptococcus that is responsible for almost all instances of tooth decay in humans. These bacteria break down sugars consumed and produce acid that wears out teeth. The wearing, in turn, becomes decay.
Research was led by Dr. Damien Brady, whose team set out to find out if the coconut oil would have an effect on the bacteria Streptococcus, which is present in virtually all human mouths. It is the Streptococcus that is responsible for almost all instances of tooth decay in humans. These bacteria break down sugars consumed and produce acid that wears out teeth. The wearing, in turn, becomes decay.