If Your Teeth Have Been Hurting Since the Snowstorm in Monroe, You’re Not Alone
Why Do My Teeth Hurt When It’s Cold?
How Winter Weather and Snowstorms Affect Your Teeth in Monroe, North Carolina
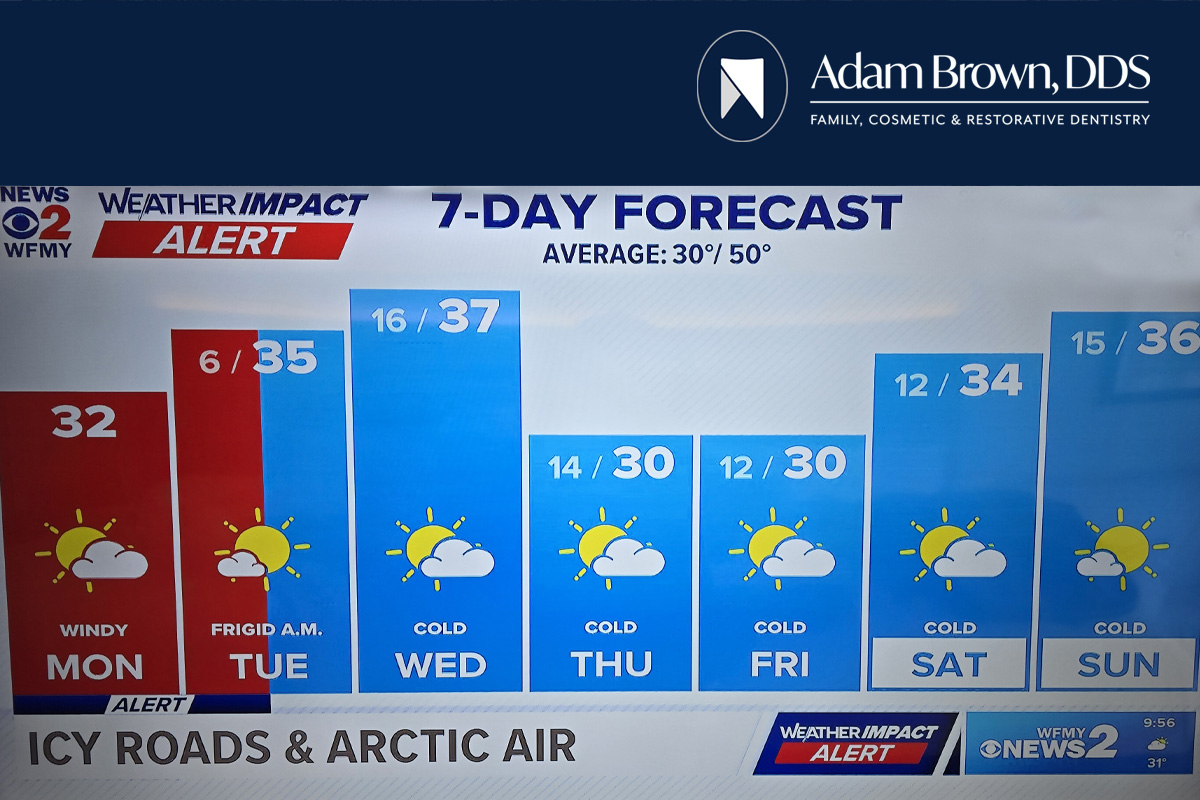
The recent snow and ice storm in Monroe, North Carolina has brought unusually cold temperatures, hazardous road conditions, and power outages across Union County. Many residents are dealing with unseasonably cold weather that is expected to linger through the week. According to local meteorologist Brad Panovich, this stretch of cold air is expected to keep temperatures well below average, with overnight lows remaining near freezing and daytime highs struggling to warm up.
How cold and snow impact your tooth sensitivity
While most people are focused on staying warm and safe, many Monroe residents are noticing something unexpected. Tooth pain and sensitivity often become more noticeable during cold weather, especially during prolonged cold spells like the one currently affecting the area.
Dentist Adam Brown of Monroe, North Carolina often sees an increase in cold related tooth sensitivity during winter weather events. Understanding why this happens and how to protect your teeth can help prevent discomfort and more serious dental problems.
Why Teeth Hurt More During Cold Weather
Tooth pain during cold weather is common and often linked to tooth sensitivity. However, cold temperatures can affect your teeth in several different ways.
Tooth Sensitivity and Exposed Dentin
Each tooth is protected by enamel, which acts as a barrier against temperature changes. Underneath the enamel is dentin, a softer layer that contains tiny tubules connected to the tooth’s nerve.
When enamel becomes thin or damaged, or when gums recede, cold air can reach the dentin. This triggers the nerve inside the tooth and causes sharp or aching pain. Cold weather makes this reaction more noticeable, especially when breathing in cold air outdoors.
Expansion and Contraction of Teeth
Teeth naturally expand in warmer temperatures and contract in cold temperatures. Rapid temperature changes can place stress on tooth enamel. Going from a warm home to freezing outdoor air during a Monroe winter storm can worsen existing cracks or weaken enamel over time.
This is especially common in teeth that already have fillings, crowns, or previous dental work.
Dry Mouth During Winter Weather
Cold air holds less moisture, and indoor heating systems dry the air even more. This often leads to dry mouth during winter.
Saliva is essential for oral health because it washes away food particles, neutralizes acids, and helps protect enamel. When saliva production decreases, the risk of tooth decay and gum irritation increases. Both conditions can contribute to tooth pain and sensitivity.
Sinus Pressure Mimicking Tooth Pain
Cold weather in Monroe often brings sinus congestion, colds, and respiratory infections. The roots of the upper teeth sit close to the sinus cavities. When sinuses become inflamed or congested, the pressure can feel like tooth pain.
Many people mistake sinus related discomfort for a dental problem, especially during prolonged cold spells.
How Winter Storms Affect Oral Health
Severe winter weather impacts oral health in ways people may not expect.
Increased Risk of Dental Injuries
Snow and ice increase the risk of slips and falls. A fall on icy sidewalks or driveways can lead to chipped, cracked, or knocked out teeth. Cold weather can also cause people to clench their jaws, increasing the risk of cracked teeth and jaw pain.
Delayed Dental Care Due to Travel Conditions
Hazardous road conditions during Monroe snow and ice storms can make it difficult or unsafe to travel. As a result, many people delay dental appointments or ignore tooth pain until weather conditions improve.
Delaying care can allow minor issues such as small cavities or gum irritation to become more serious problems.
Disrupted Routines During Power Outages
Power outages and disrupted schedules can interfere with daily routines, including oral hygiene. Skipping brushing or flossing for even a short time can allow plaque to build up, increasing the risk of tooth decay and gum disease.
Stress and Teeth Grinding
Winter storms often cause stress and anxiety. Concerns about power loss, cold temperatures, and travel safety can lead to jaw clenching or teeth grinding. This can cause headaches, jaw pain, worn enamel, and increased tooth sensitivity.
Dental Care Tips During Winter Storms in Monroe, NC
Even during severe weather, protecting your teeth is important. Dentist Adam Brown recommends the following steps to help Monroe residents maintain good oral health during cold weather events.
Maintain a Consistent Oral Hygiene Routine
Brush your teeth at least twice a day using fluoride toothpaste and floss daily. If power outages disrupt routines, rinse with water until brushing is possible. Keeping plaque under control helps prevent sensitivity and decay.
Protect Teeth From Cold Air
Covering your mouth with a scarf or face covering when outdoors can help reduce exposure to cold air. Breathing through your nose rather than your mouth can also reduce discomfort for sensitive teeth.
Stay Hydrated
Drink plenty of water throughout the day to prevent dry mouth. Staying hydrated helps maintain saliva production, which protects tooth enamel and reduces sensitivity.
Avoid Chewing Ice
Chewing ice can crack teeth, damage fillings, and worsen sensitivity. Teeth are already stressed during cold weather, so avoiding ice is especially important.
Limit Rapid Temperature Changes
Switching quickly between hot foods and cold air can increase tooth discomfort. Try to allow foods and drinks to cool slightly before consuming them, and avoid exposing your teeth to sudden temperature shifts.
Manage Stress and Jaw Clenching
Be mindful of jaw tension during stressful moments. Relaxation techniques and gentle jaw stretching can help reduce clenching. If grinding is a frequent issue, a dentist may recommend a night guard.
When Cold Weather Tooth Pain Should Be Checked by a Dentist
Cold weather often exposes underlying dental problems rather than causing them. You should consider seeing a dentist if you experience persistent or worsening pain.
Warning signs include sharp pain when exposed to cold, pain when biting or chewing, swelling in the gums or face, bleeding gums, or tooth pain that does not improve when temperatures rise.
These symptoms may indicate cavities, cracked teeth, gum disease, worn enamel, or failing dental restorations.
Dental Emergencies During Winter Weather
Some dental problems require prompt attention even during winter storms. These include severe tooth pain, broken or knocked out teeth, swelling or abscesses, and uncontrolled bleeding.
If travel is unsafe, contact a dental office for guidance until conditions improve. Dentist Adam Brown and his team can provide instructions on how to manage dental emergencies until in office care is possible.
Preventing Winter Tooth Pain With Regular Dental Care
Routine dental visits help identify problems early and reduce the risk of winter related tooth pain. Professional cleanings and exams help detect enamel wear, early cavities, and gum recession before they cause discomfort.
For Monroe, North Carolina residents, staying proactive with dental care helps protect oral health during extreme weather and throughout the year.
Final Thoughts for Monroe, North Carolina Residents
The recent snow and ice storm has brought challenges for many families in Monroe. Cold weather affects more than roads and power lines. It can also impact oral health.
If your teeth hurt more when it is cold, the discomfort may be related to sensitivity, enamel wear, dry mouth, sinus pressure, or stress. Paying attention to these symptoms and practicing good oral hygiene can help protect your smile during winter weather.
If tooth pain persists or worsens, scheduling a dental evaluation with Adam Brown DDS can help identify the cause and prevent further complications once travel conditions improve.
Frequently Asked Questions
Why do my teeth hurt when it is cold outside?
Cold air can reach sensitive areas of the tooth when enamel is worn or gums have receded. This triggers the tooth’s nerve and causes pain.
Can cold weather cause permanent tooth damage?
Cold weather itself does not damage teeth, but it can worsen existing problems such as cracks, cavities, or enamel erosion.
Why does my tooth pain get worse during winter storms?
Dry air, stress, sinus pressure, and changes in routine during winter storms can all contribute to increased tooth sensitivity and pain.
How can I protect my teeth during cold weather in Monroe, NC?
Brushing and flossing daily, staying hydrated, covering your mouth outdoors, and avoiding chewing ice can help protect your teeth during cold weather.
When should I see a dentist for cold related tooth pain?
You should see a dentist if tooth pain is persistent, sharp, or accompanied by swelling, bleeding, or pain when chewing.
Disclaimer
This article is for educational purposes only and is not a substitute for professional dental advice. Always consult a licensed dentist for diagnosis and treatment recommendations.