Your Teeth as You Age – Adam Brown, DDS
Your Teeth as You Age
Every new day brings in an older and wiser version of ourselves. But we don’t just become wiser; our bodies change too. Teeth are especially prone to change and incur wear over time, something that older readers may have already experienced.
In fact, nearly 1 in 5 adults over the age of 65 are missing all of their teeth — a testament to how the evolution and rapid change of our tooth health can lead to real dental damage.
As you age, the increased likelihood of dental problems is nothing to ignore. And with age introducing new problems and concerns, some people can see a lifetime of care for their teeth seemingly evaporate in months.
“You have people who have maintained their oral health their entire lives, only to see it go down the tubes in six to eight months,” – Judith Jones, Professor at Boston University’s dental school and elder-care spokeswoman for the American Dental Association.
While there are a number of causes for the increased risk in older teeth, the overall change in your teeth is most to blame. Teeth soften as we age, increasing challenges and risks, among other changes.
So don’t leave your aging teeth to fight for their health alone; schedule an appointment with a qualified dentist today to preserve dental health and stay healthy for the long run. And there’s no better dentist to go to for that type of preventive care than Adam Brown DDS. Years of experience helping older patients in the Monroe area equip this office to provide the best care for aging teeth.
What Makes Our Teeth?
Most people believe that our teeth are an extension of our bones — but that’s a common misconception. It’s likely rooted in the fact that your teeth and bones mostly comprise calcium. Additionally, much like our bones and joints, a lifetime of use can create pain and damage, especially if left untreated. While they have these things in common, the two have unique differences.
Bones are living tissue – teeth are not. Most readers know that bones can heal and repair themselves, but teeth can not. This means preservation and additional care are key to having teeth that can stand the test of time. Teeth have four different types of tissue, all of which can experience changes or damage with age:
Enamel – Your enamel forms the outer layer of your teeth, protecting the more sensitive inner parts of your tooth from damage Enamel is the strongest substance in your body, so it plays its role as a protector well.
Over time, your enamel is prone to erosion, opening up gaps in protecting your teeth. And because these cells aren’t living, the cracks formed are permanent. Additionally, this layer is the part of your teeth that can stain, leading to discoloration.
Dentin – Dentin is the layer wedged between your enamel and cementum. Dentin serves a similar role to enamel, protecting the crown of your teeth. Still, it is much softer than enamel, so it can develop decay and cavities rapidly, especially if left untreated.
If there’s been a specific part of your mouth causing you discomfort, it could be the case that your dentin is taking a beating. If that’s the case, it’s important to schedule a check-up with a dentist right away!
Cementum – Cementum is a substance covering the root of your tooth. It connects your teeth to the gums and is softer than both dentin and enamel. This and the next layer are important to keep protected, as damage or decay to these components could spell real problems.
Pulp – Also known as the nerve in your tooth, this layer has blood tissue and nerves that connect your teeth to the rest of your body. Often, we talk about how dental health plays a role in your overall health. If you need an example of this, look no further than the pulp, which plays a bridge between oral and overall health.
The Factors that Change Our Teeth
Still, why are our teeth more prone to damage and disease when we age? There’s no singular answer to this, but rather a number of factors that create an overall more vulnerable oral health for older patients.
Wear and Tear
The longer you use something, the more wear and tear it will go under — this is true for your teeth, too!
Daily use over the course of years can damage your teeth, erasing enamel, an important layer for healthy teeth! Teeth are also more likely to crack or break with age, so avoid hard foods or ice to ensure longevity. Those with enough wear and tear may consider crowns or veneers, both offered by Adam Brown DDS.
To prevent some of the more severe impacts of dental wear and tear, you could try and chew your food evenly. Some people chew with specific parts of their mouth, which compounds the risk of overuse and damage.
Dry Mouth
According to studies by the National Library of Medicine, over 46% of those over the age of 65 experience dry mouth.
Countless medications have side effects that contribute to dry mouth, which could be a cause in this large number of affected people. While dry mouth creates discomfort, you may be surprised at the damage it can cause to your teeth. Saliva is important in fighting off bacteria growth, contributing to tooth decay. Look to switch medications if the issue persists, or drink more water to prevent your mouth from getting too dry.
Overeating and Drinking Certain- Foods
While most foods in moderation won’t impact your teeth negatively, a lifetime of consumption can create real problems. Foods high in acid spell trouble for your enamel, especially if used consistently over the course of years. Other foods that create stains, like coffee and red wine, can lead to real discoloration and a less polished smile.
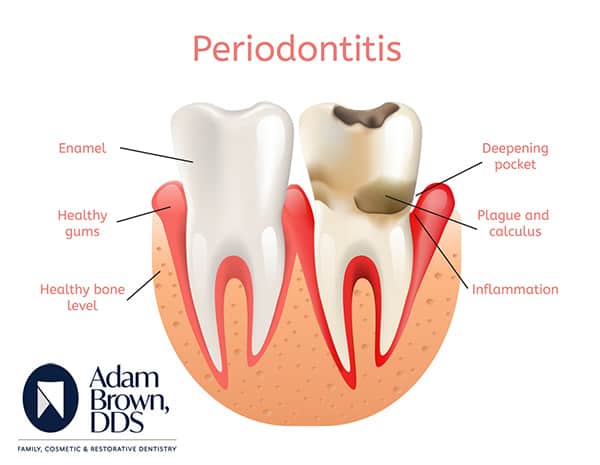
Maintaining a Strong Support System – Your Gums
Your teeth aren’t alone in oral hygiene. Your gums are an important part of keeping your oral health in check. Gum disease that leads to a receding gumline exposes your teeth to more damage, increasing risks of disease and problems.
“Age itself isn’t a cause, but the periodontal disease often slowly gets worse and goes undetected — and untreated — for decades, leading to more severe problems in the seventh decade of life and beyond.” – Harvard Health Publishing.
As the researchers at Harvard Health Publishing said, if untreated, you’ll encounter severe problems ranging well beyond just your tooth health. Adam Brown DDS offers periodontal treatment that will give your teeth the strong supporting cast they deserve for a healthy life.
The Role of Ongoing Preventative Care
While knowing the factors and what to avoid can prevent some damage, few things are more effective at keeping your teeth healthy than consistent and ongoing preventative care. Many wait until a problem is unignorable to make the jump to schedule a dental appointment, but at that point — irreparable damage could have already happened, squashing a lifetime of care and attention to your teeth. Even worse, a lot of our elderly population is experiencing gaps in care during an important time for checkups and treatment.
“Medicare does not cover routine dental services. Nearly 24 million Medicare beneficiaries lack critical oral health coverage, six meaning many older adults do not receive regular dental services.” – Johnson, Dental Economics.
With new patient specials and an office dedicated to getting you the help they need, Adam Brown DDS is looking to tackle this gap and provide those who need care with best-in-class treatment options. So, don’t hesitate to call and explore your options!
A Dentist Who Understands
We all know that aging creates problems, but having a patient and understanding dentist who’s ready to face those challenges alongside you is necessary to reverse the trends of poor senior dental health across the country. Reviews of Adam Brown DDS echo just that —
“Dr. Brown was friendly and very accommodating. He is honest in his dealings and tries to work with patients’ situations. My parents are both elderly with various health issues that can make visits difficult for both patients and doctors. He has been kind and patient with them. They love him!” – Google Review for Adam Brown DDS.
With the right care and preventative treatment, you can keep the teeth of your youth and have a much healthier mouth and body in turn. Schedule an appointment with Adam Brown DDS today and see about starting a new journey for positive dental health — even after the seventh decade!





 Signs of Gingivitis and Periodontal Disease
Signs of Gingivitis and Periodontal Disease