Are You Prepared For A Dental 911 on Vacation?
What To Do if You Have a Dental Emergency While on Vacation
As unpredictable as life can be, it’s worth preparing for certain emergencies, especially when traveling away from home. Obviously, with the hope no emergency comes about. Keeping a first-aid kit in your car; setting a security alarm on your home; even bringing an extra set of clothes are examples of our preparedness, but there’s another situation that is often forgotten: a dental emergency. Do you know what to do if you or a loved one has a dental mishap while traveling or on vacation?

Picture yourself on a beach. You can hear the waves moving out and coming back in — that soft, loud rush of sound that works as a charging station for the mind, body, and soul. Now see yourself reaching to the side of your chair to grab your favorite beachy drink, and as you go for a sip…you clink the edge of the class to your tooth and your tooth chips! It can be that easy, and it can be that quick. And without a plan, this sort of emergency can only get worse.
No matter where you are or what you’re doing, an unexpected toothache, broken teeth, and general mouth pain can happen, but that doesn’t mean you have to suffer. Most likely, unless you are truly off the grid, you should be able to find care nearby.
Worst case, you end up in the emergency room and leave with a prescription for pain medication that can get you in the clear until you’re back home. But this can be expensive, and it doesn’t diagnose or solve the issue. It alleviates it and pushes it down the road for later. Adam Brown, DDS explains some of the most common dental emergencies and how to respond to them:
Common Types of Dental Emergencies
If you can imagine the emergency, it can most likely happen. With that in mind, the following are the most typical dental emergencies:
- A tooth or multiple teeth fall out due to chewing something hard or taking a blow to the mouth.
- You lose a crown or filling from chewing ice, hard candy, etc.
- You injure your gums, palate, or mouth by taking some sort of impact to the face.
- A tooth becomes loose.
- You chip or fracture a tooth. (Maybe from misjudging the distance between your mouth and your favorite beachy drink.)
- You feel sudden, unusual, excruciating pain inside the mouth. This could be the roots of the teeth, the gums themselves, etc.
- Your gums or mouth starts to swell and change color (deep red or grey/white).
How does one respond to any of these tragedies? In a number of ways. It depends on your exact situation: how threatening the injury is, who is with you, where you are in proximity to getting help.
But one thing to keep in mind is that if you do lose a tooth: immediate action needs to be taken, as the amount of time a tooth is absent from the gums and root system determines the likelihood of a dentist being able to successfully replace it.
How to Respond When a Dental Emergency Happens
Whether or not the dental emergency is yours or not, it’s good to be prepared to handle what could be thrown your way. Here are a couple of those common emergencies along with some commentary on how to respond:
A Toothache and/or Mouth Pain
Such a severe, sharp pain as what’s experienced in this situation can constitute an emergency. What can be tricky about oral pain is that, a lot of times, it begins with a dull pain that seems insignificant. That is until it begins to throb.
Here is what to do: First, examine your mouth to make sure there is no visible source of the pain. If there isn’t, look for discoloration or swelling. If you see either, it’s a good idea to find a doctor or dentist to give it a look. Otherwise, if it’s only a dull pain, take over-the-counter pain medicine until you can reach a dentist.
A Broken, Cracked, or Dislodged Tooth
This can happen due to sport, play, or a freak accident. And, no matter the reason for a broken or chipped tooth, an immediate trip to an emergency dentist or the emergency room will be necessary.
It’s a good idea to research a local (to where you will be) dentist and find the contact information and hours of operation. If you know you’ll be active on your trip — and that a dental emergency is possible — consider contacting the dentist to see if she (or anyone she knows) can be of assistance in case of an emergency.
This might seem like a bit much. But due to the commonality of dental emergencies while traveling, and the fact that you like your teeth and would like to keep them intact, it’s smart to plan for the worst.
*Note: If you do lose a tooth, rinse your mouth with cold water and apply a cold compress to the area where the tooth is missing. This will help control inflammation until you can get proper aid.
Prepping for Your Trip
The following are a few quick tips for when you’re preparing for a trip:
- Locate your dental and medical insurance documents and give them a thorough reading, as to see what sort of coverage you have while traveling.
- For any and every place you plan to visit, locate their medical facilities so you know where to go if something were to happen — dental emergency or otherwise. Be sure to record the pertinent information so you have it readily available.
- If you’re having any sort of pain or oral issues prior to leaving for your trip, schedule a thorough checkup before leaving. Also, mention your plans to your dentist to confirm he recommends travel while in your specific condition.
- Always pack pain medicine and oral hygiene products so you can do as much as possible for your oral care yourself while out and about.
- Be cognizant of your oral condition while traveling. Consider keeping from hard chewing that could potentially damage your teeth and/or gums (e.g., hard candies, ice, etc.).
- If you’re going to play a sport, or you plan to become physically active while on vacation, bring a protective mouth guard to keep your teeth and gums safe.
Finding a Dentist While Traveling
Remember that you’re planning for something that hopefully won’t happen, so you don’t want to expend too much time and energy on this. But you do want to be thorough enough so you’re prepared if anything does happen.
Take 30 minutes to research a local dentist; then, send an email or give them a call. Even if they don’t offer services when you need them, they might be able to point you to someone who does. Worst case scenario, go to the emergency room.
No matter how things pan out while on your trip, if you do have an emergency and you receive emergency care, make it a priority to visit your home dentist as soon as you return. And most importantly, don’t forget to have fun!





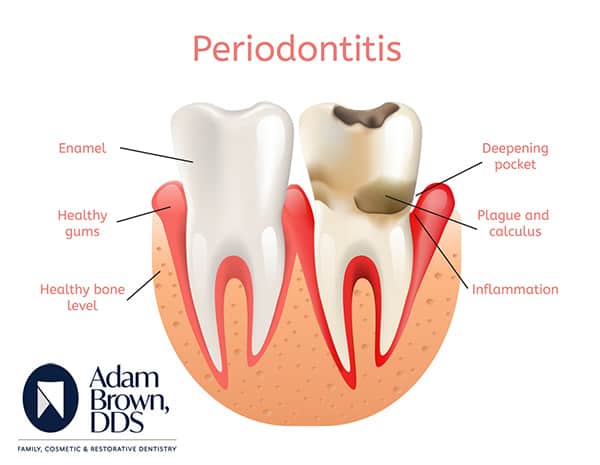 Signs of Gingivitis and Periodontal Disease
Signs of Gingivitis and Periodontal Disease