8 Ways to Sustain Your Family’s Dental Hygiene This Summer

Summer is around the corner, which means it’s time for all the fun things that come with Summer. Maybe your family is planning to go on a big vacation. Maybe you’re getting geared up for long days at the pool. Perhaps you’re looking forward to some sweet, cold treats to tame the rising temperatures.
But amid the summertime excitement, it’s important not to leave your dental health in the dust. The shifts in routine and the seasonal activities don’t remove your family’s need to maintain good oral hygiene habits. Adam Brown DDS is here with some practical tips and information for how your family can keep your teeth and gums healthy through the sun-kissed days of Summer:
- Stick to Your Dental Routine
We’ll start with the basics: keeping up with your normal dental care routine. Even if your kids are out of school and staying up later than usual, don’t let them go to bed without brushing their teeth. And to the adults in the room—don’t allow yourselves to get lax either!
For many families, summer is packed with special events and relaxed bedtimes, but everyone should be brushing twice a day for two minutes with fluoride toothpaste. Also, make sure you are flossing once a day; any two teeth that touch should be cleaned regularly. Many children lack the motor skills to floss until they are more than 10-years-old. If necessary, help your child floss, or invest in a water flosser.
- Pack Wisely
The quickest way for your family to fall behind on dental hygiene is to forget the essentials when you travel. As you plan your vacation, be sure to pack travel-sized items like these:
Toothbrush
Like the other items on this list, you can find a selection of travel-sized toothbrushes at most major retailers, grocery stores, and pharmacies. These brushes will fold and easily fit into a carry-on bag. Your travel brush may not be quite as comfortable or effective as your full-sized brush, but it will get the job done.
Toothpaste
Fluoride toothpaste is another essential item that you can’t go without on your trip. If you only took two dental care products when you travel, you would want them to be a toothbrush and toothpaste.
Floss
You can get travel-sized packs of floss, but flossers are even better. Particularly if you have kids, flossers are easier to use on the go, and they’re effective at removing excess food particles and plaque between teeth. If possible, bring a pack of floss in addition to your flosser.
Mouthwash
While it shouldn’t be used to replace your brushing habit too often, mouthwash can do wonders for killing bacteria and germs in your mouth. You won’t have any trouble fitting travel-sized mouthwashes in your carry-on, and you can use them to freshen your breath when you don’t have a chance to brush.
Toothpicks
Toothpicks are the perfect little gadgets for removing food particles after a meal. Get a travel-sized pack of toothpicks for your trip to use when you don’t have the opportunity to floss.
Wisps
Manufactured by Colgate, Wisp brushes are relatively new. And they’re one of the handiest oral hygiene products you can buy. These pocket-sized, disposable brushes are surprisingly effective at removing food particles and plaque, and each brush comes with a built-in freshening bead that releases toothpaste as you brush. The best part is that you don’t even have to rinse!
Sugar-Free Gum
Chewing gum is great for keeping bad breath at bay, but it also increases saliva production when you chew it. Since saliva is essential for dissolving acids and helping you fight dry mouth, this is a good thing. Stay fresh and avoid cavities by packing sugar-free gum for your vacation.
- Consider Sustainable Products
While travel-sized dental care products are great for taking trips, using eco-conscious products for your everyday routine is a great way to benefit both your oral health and the environment. Here are some of the most popular types of eco-conscious dental care products available today:
Toothbrushes
Plastic toothbrushes typically are not compostable, nor are the packages they come in. That’s why bamboo toothbrushes are gaining in popularity. Not only are the bristles and handles easily compostable, but bamboo brushes can be just as effective for cleaning your teeth and gums as conventional brushes.
Toothpaste
Natural toothpaste has been around for a long time. But it has come a long way over the years in terms of helping you effectively remove plaque and prevent cavities. Unless you have a high decay risk, your family could benefit your oral health and the environment by using natural toothpaste that comes in a compostable tube.
Floss
The packaging of conventional floss can take years to biodegrade. There are many sustainable, low-waste floss products on the market that come in biodegradable packaging and are just as effective at removing food particles and plaque.
Mouthwash
Alcohol-based mouthwashes may leave you with a feeling of freshness in your mouth, but they can also dehydrate your oral cavity, hinder saliva production, and cause irritation. If you want to add a mouth rinse to your dental care routine, opt for one that contains coconut oil and xylitol, which are known for their antibacterial properties and less harsh on the gums than alcohol.
Whitening
Brushing with a mixture of hydrogen peroxide and baking soda once a week can noticeably brighten your smile, and it has no impact on the environment! Just make sure it’s not part of your daily routine. When used too frequently, hydrogen peroxide can cause chemical burns on your gums while baking soda can damage your enamel.
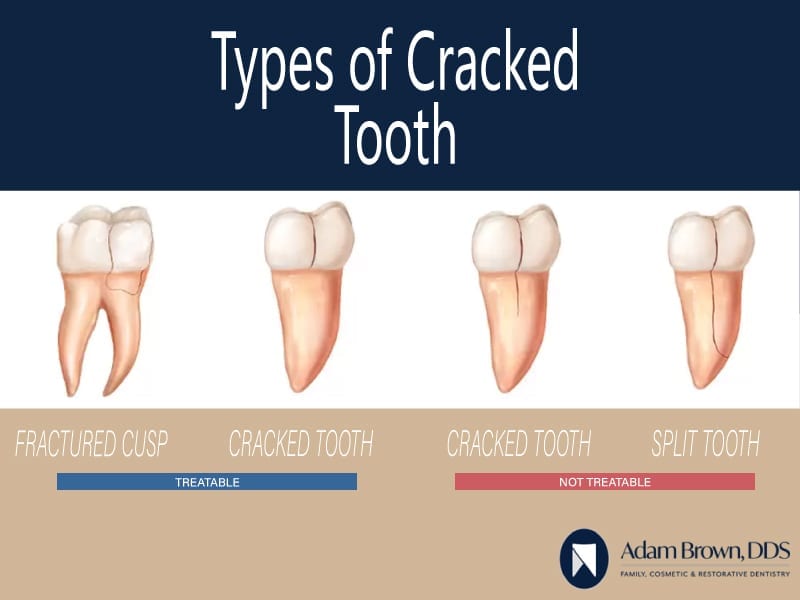
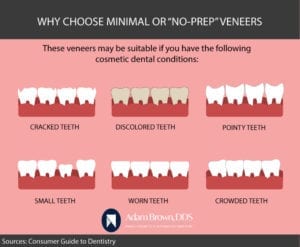
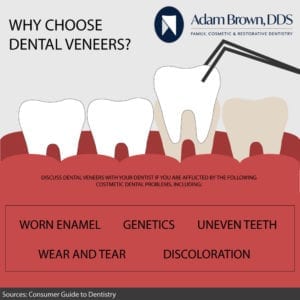
- Don’t Chew Ice
Few things are more satisfying than an ice-cold drink on a hot summer day. But if you’re an ice-chewer, know the risks that come with it. Chewing ice, especially large cubes, can cause a variety of oral health issues and even lead to a hefty bill from the dentist or orthodontist. Some common consequences of chewing ice include damaged tooth enamel, damaged dental fillings, cracked or chipped teeth, and broken oral appliances.
While adults should also take precautions, kids are particularly prone to chew ice subconsciously. Make sure your children know the risks involved and try to prevent the habit if possible. If anyone in your family experiences one of the injuries above to your teeth or oral appliances, contact Adam Brown DDS immediately to arrange an emergency dental visit.
- Limit Sugary Foods and Drinks
We get it—Summer is meant to be enjoyed. And sometimes that includes chomping on yummy foods that are not so good for your teeth. Try to moderate your consumption of sugary foods and beverages, as they can significantly hinder your oral health routine. For example, sodas, juices, and ice cream can erode your enamel and cause cavities. Even acidic fruits like blueberries and pineapples can harm your enamel. After eating foods like these, be sure to rinse your mouth, brush, and floss as soon as possible.
- Embrace Healthy Summer Foods
Now that you have an idea of what foods to limit in your summer diet, let’s talk about some foods that can specifically benefit your oral health:
Salmon
Salmon is not only a versatile fish for recipes, but it’s also one of the best foods you can eat for vitamin D. And without vitamin D, your body won’t be able to absorb nutrients like calcium. Salmon is also an excellent source of omega-3 fatty acids, which are critical in the prevention of periodontal disease and fostering overall health.
Cheese
For most people, this one doesn’t take a lot of convincing. Obviously, cheese is best eaten in moderation because it’s high in fat content, but it’s a wonderful source of calcium. And calcium is perhaps the single most beneficial nutrient for teeth, as it helps to keep your enamel strong and your jawbones durable. Moreover, cheese contains casein—a protein that provides a protective layer on your teeth and helps prevent tooth decay.
Bananas
Bananas are one of the most beneficial fruits you can eat for your dental health. They have a low acidic content, and they’re high in potassium, which helps to maintain jawbone density and tooth strength. Yes, bananas have sugar in them, but they won’t stick to your teeth like candy and other sugary foods.
Oranges
Vitamin C plays a critical role in helping your gums fight off gingivitis and other oral infections, and oranges offer a beaucoup of vitamin C. Boost your gum health, and you’ll significantly lower your risk of loose teeth.
Apples
If nature had a toothbrush, it would be an apple. Along with containing vital nutrients (e.g., potassium, vitamin C, fiber, etc.), apples massage the gums, increase saliva, and remove plaque. Making apples a part of your daily diet will help you maintain a clean mouth, fresh breath, healthy gums, and strong teeth.
Carrots
Carrots are also a wonder for cleaning your teeth and gums. They contain lots of keratin, which combat plaque and tartar, and they massage your gums. They also have beta carotene, a nutrient that converts to vitamin A, which increases saliva production and enables oral wounds to heal more quickly.
Kale
This superfood is known for its incredible array of nutrients, and it’s one of the best foods you can eat for your oral and overall health. Kale has high levels of vitamin K, which helps to protect your bones and enamel, boost your immune system, and foster healing. It also helps the body absorb osteocalcin—another nutrient that benefits bones and teeth.
- Drink Plenty of Water
Water is essential for keeping you hydrated in the heat. But it also comes with specific dental benefits. For instance, it helps to keep your mouth clean by washing away leftover food and residue that would otherwise attract bacteria, in turn reducing the risk of cavities. Furthermore, water dilutes the acids produced by oral bacteria. Start your morning off with a glass of water, and always keep a refillable water bottle with you so that you can sip throughout the day.
- Prepare for Accidents
Finally, accidents happen. While you want to take every precaution, such as having your child wear a mouthguard while playing sports, you may not always be able to avoid injury. That’s why it’s essential to prepare a kit of supplies for your child to keep nearby in the event of a dental emergency. Whether they’re playing a contact sport, engaging in an individual physical activity, or hanging out at the pool, make sure they have easy access to a kit with these items:
- Gauze
- Saline solution
- OTC pain medication
- A small container (for a knocked-out tooth)
- The number to their dentist
Conclusion
Summertime may be when the living’s easy (especially for kids), but your family’s dental health still matters. Along with maintaining your regular oral hygiene routine, look for new products that can benefit your smile and the planet. Avoid chewing ice, consume sugary foods and beverages in moderation, and incorporate dental-friendly foods in your diet. Lastly, be sure to drink a lot of water, stay prepared for dental emergencies, and book your back-to-school appointments now at Adam Brown DDS!




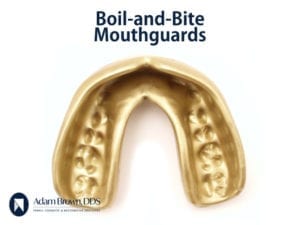
 of your teeth and fabricate a mouthguard to the exact specifications of your teeth and mouth structures. Kids who play sports regularly can greatly benefit from custom mouthguards, as can adults who deal with snoring or sleep apnea.
of your teeth and fabricate a mouthguard to the exact specifications of your teeth and mouth structures. Kids who play sports regularly can greatly benefit from custom mouthguards, as can adults who deal with snoring or sleep apnea.