COVID Is Cracking Teeth: How to Keep it from Happening to You
Cracked teeth are common. If a cracked tooth is left untreated, it can lead to physical ailments like severe pain, discomfort, and infection, not to mention a slew of mental health issues (e.g., stress, anxiety, low self-esteem, etc.). The most serious cases may even require the extraction of a tooth.
While cracked teeth have always been common, they’ve become even more so in the COVID-19 era. Dentists across the country (and the world) have noticed a significant uptick in cases. Many dental offices are experiencing an increase of about 30% in cases, while others are exceeding a 500% increase on some days. That’s right, 500%!
Let’s put that into perspective: If dental offices treated one fractured tooth per day before COVID came around (which was pretty normal), some of those offices are now seeing five cases each day. Whew, that’s a big change.
So, what’s behind the rise in cracked tooth cases? Below, we’ll answer this question and discuss the different types of cracked teeth, how to know when you should see your dentist, how you can prevent a cracked tooth from happening or worsening, and much more.
WHY THERE ARE MORE CASES OF CRACKED TEETH
No, COVID-19 doesn’t directly cause cracked teeth. However, the general rise in stress and anxiety brought about by the pandemic is considered by many medical experts to be the primary culprit for the uptick in cracked tooth cases. In short, when you’re stressed, you’re more likely to brux your teeth. Bruxism refers to the act of grinding or clenching your teeth, and over time, the pressure of bruxing can lead to cracked teeth, as well as muscle pain in the head and neck.
There are numerous concerns that the average American is dealing with during these challenging times. Along with the fear of contracting the coronavirus (for themselves and/or their loved ones) and dealing with overarching medical issues, many people are navigating significant changes in their job demands, finances, and social lives.
If it sounds like a reach to say that these stressors can lead to cracked teeth, keep in mind that bruxism was a common condition before the COVID-19 pandemic reared its ugly head and that it’s only becoming more common. And a lot of people don’t realize when they are bruxing their teeth. Actually, some dental health professionals estimate that about half of their patients are unaware that they grind or clench their teeth. This is because most bruxing happens during sleep—when you’re not fully conscious and able to relax your muscles.
Besides bruxism, there are other common causes of cracked teeth to be aware of. These include eating hard foods (e.g., nuts, hard candy, ice, etc.), getting large dental fillings that can weaken the integrity of a tooth, and subjecting your mouth to extreme temperature changes, such as burning your tongue with hot food or liquid and drinking ice water to cool it down. Also, physical trauma to the mouth—such as a sporting injury, automobile accident, or fall—can cause teeth to crack, as can age (most cases are in people 50 or over).
THE DIFFERENT KINDS OF CRACKED TEETH
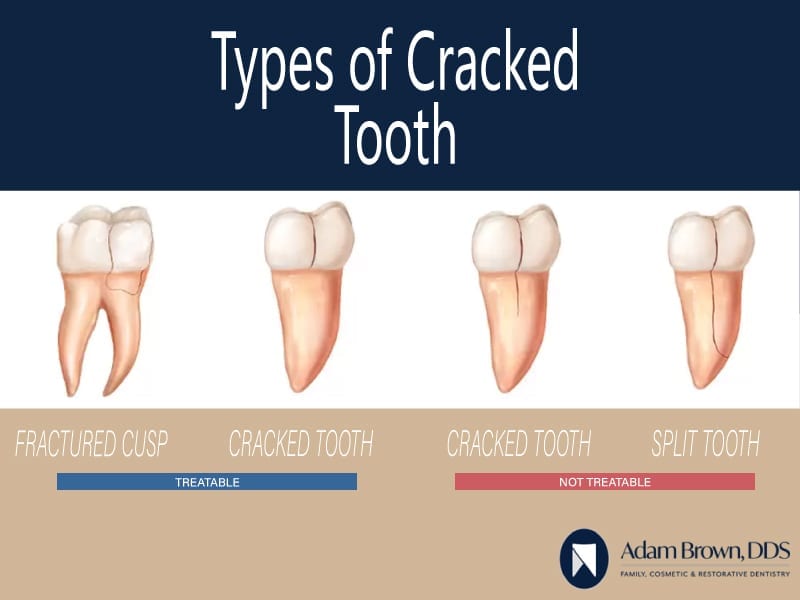
According to the American Association of Endodontists (AAE), there are five types of tooth cracks/fractures, all of which vary in severity and treatment possibility/requirements:
- Craze lines
- Fractured cusp
- Cracked tooth (extending to the gum line)
- Split tooth
- Vertical root fracture
Knowing about these different types can help you to better identify issues and determine what steps to take when you experience certain symptoms. Here’s a little detail on each type of cracked tooth:
Craze Lines
This is the most common and least severe type of cracked tooth. In fact, all teeth have craze lines, which are essentially micro-cracks in the enamel. Since these cracks don’t reach the dentin (the tissue beneath the enamel) or cause pain, no treatment is necessary.
Fractured Cusp
Another type of cracked tooth that generally doesn’t cause pain is a fractured cusp. This typically occurs when a patient has a dental filling and the surrounding area of the tooth undergoes a small fracture. A fractured cusp doesn’t impact the pulp (the tooth’s center that holds the nerves, blood vessels, and connective tissue), which is why it’s usually painless. In most cases, crowning can fix a fractured cusp.
Cracked Tooth (Extending into the Gum Line)
When a tooth has a vertical crack all the way through but it doesn’t enter the gum line, it’s typically savable through bonding or crowning. But treatment options become murkier if the crack has extended into the gum line. At that point, it really depends on how far into the gum line the crack has grown. Consulting a dentist and acting quickly is the best way to save the tooth; if too much time passes, extraction may be necessary.
Split Tooth
Going a step further, a split tooth is when a crack has extended well into the gum line—enough to where the tooth can be divided into two segments. If you have a split tooth, chances are you will not be able to save the whole tooth, but your dentist might be able to preserve a portion of the tooth. Again, the faster you act, the better your chances are for avoiding extraction.
Vertical Root Fracture
This is the most severe type of cracked tooth. A vertical root fracture grows upward, from below the gum line through the top of the tooth. The prognosis for a vertical root fracture is generally not good; in most cases, the entire tooth will need to be extracted.
SYMPTOMS, DIAGNOSIS, AND TREATMENT
Sometimes, people are not able to tell when they have a cracked tooth, particularly in the early stages. Obviously, this is unfortunate because it can hinder you from seeking treatment early on. But oftentimes, there will be symptoms, and it’s important to know what to look out for.
For instance, if you notice a heightened sensitivity to temperatures or sweetness when eating or drinking, or if your gums are swollen around a particular tooth, it could be a sign of a cracked tooth. Also, if you experience pain while biting or chewing, it’s essential to get checked out by a dentist, even if the pain is inconsistent. Most pain from a cracked tooth comes with the release of biting pressure.
When it comes to the diagnosis process, it can help to know what to expect. Though x-rays can reveal poor pulp health (which can indicate a crack), they often don’t actually show cracks in teeth. Therefore, your dentist is likely to take several other steps to get to the bottom of things, such as:
- Going over your dental history (do you regularly eat hard foods or clench/grind your teeth?)
- Using a magnifying lens to examine your teeth for cracks.
- Using a dental explorer on your teeth to feel for cracks.
- Applying dental dye, which can reveal cracks.
- Asking you to bite down on something in order to pinpoint the pain.
- Examining your gums for inflammation.
There are four primary forms of treatments for a cracked tooth. The one that is best for you will depend on the crack’s location and the extent of the damage wrought:
Bonding. In mild cases, a dentist can use bonding to fix a cracked tooth. This process includes applying a plastic resin to fill the crack, which can help the tooth to look and function like normal for years to come.
Crowning. Porcelain or ceramic crowns are used to either fit over or cap a cracked tooth. To make this prosthetic device, your dentist will probably need to make an impression of your tooth and send it off to a lab that will manufacture the crown. The dentist will also need to take a little enamel off of your tooth so that the crown will fit properly.
Once the crown comes back from the lab (usually in a couple of weeks), the dentist will fit the crown over your tooth and use cement to permanently bond it. Crowns can last a lifetime when taken care of properly.
Performing a root canal. If your tooth crack has reached the pulp of your tooth, you may be advised to get a root canal. This procedure is typically performed by a dentist, oral surgeon, or endodontist, and it involves the removal of damaged pulp. By reestablishing some integrity in the tooth, a root canal can help you avoid further weakening or infection.
Extracting. This is the last resort. But when a tooth crack is severe enough, removing the tooth can help you prevent a whole host of other health problems. Your dentist might recommend extraction if there is simply too much damage done to the tooth’s structure, nerves, and roots.
HOW TO PREVENT BRUXISM
So, now that you know that bruxism is the leading cause of cracked teeth, how do you keep yourself from grinding and clenching your teeth? Well, there are some practical steps you can take each day to prevent bruxism or at least mitigate its effects.
For example, incorporate stress-reducing activities into your routine, such as exercise, yoga, meditation, acupuncture, and/or massage. Try to maintain proper posture when sitting (especially while working), as an aligned spine and relaxed jaw can reduce clenching. Be aware of how you’re holding your jaw during the day; remember that your teeth should not be touching unless you’re eating or speaking.
If you notice your teeth clenching, start placing your tongue between your teeth. The sensitivity of your tongue will encourage you to stop clenching. When it comes to bruxing during sleep, which is when it most often happens, look into products that can help. For instance, wearing a night guard can prevent your teeth from touching, even if you’re subconsciously grinding and clenching. And research the various customized pillows and neck positioners on the market that can relieve stress and pressure from your jaws and neck during sleep.
THE IMPORTANCE OF GOING TO THE DENTIST
If you notice any of the symptoms mentioned above, or if anyone else in your life notices that you’re bruxing your teeth, it’s essential to contact your dentist right away. The quicker you respond, the greater the chances that you will be able to fix the problem before it gets to the point of extraction. Dental offices across the country, including Adam Brown Dentistry, are taking painstaking precautions to keep patients and staff members safe during the pandemic, so don’t hesitate to make an appointment today!
PRACTICING DENTAL HYGIENE AT HOME
Finally, as with any other dental/oral health issue, one of the best ways to prevent cracked teeth is to practice daily dental hygiene. Be sure to brush twice a day, floss once a day, and use mouthwash regularly. Also, be conscious of your diet, as the foods and drinks you consume can have a significant impact on your dental health.
The COVID-19 pandemic has profoundly affected the lives of countless Americans in many ways—one being that more people are experiencing cracked teeth. Continue to practice good dental hygiene each day, take any necessary steps to prevent bruxism, and be on the lookout for any symptoms that could indicate a cracked tooth. And of course, call Adam Brown Dentistry today to schedule an appointment!